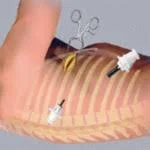
Video-Assisted Thoracic Surgery (VATS) or Thoracoscopy
In the past, chest surgery required a large incision and a week-long hospital stay. VATS offers another option, a “minimally invasive” TECHNIQUE. It allows surgeons to view the inside of the chest cavity using a thin scope and small incisions. VATS is used most often to:
- Find the cause of lung problems
- Drain fluid from around the lung
- Remove or biopsy chest tumors
- Help prevent build-up of fluid in the chest (Pleurodesis)
After VATS, patients have:
- A faster recovery
- Shorter hospital stay
- Less pain
With VATS, the risk for bleeding and infection are low. You will have a drainage tube from your chest after surgery that is removed before you go home. Sometimes, the tube has to stay in longer than one day, which may increase your hospital stay.